Fertility Questions
Are you overwhelmed by the fertility information on the internet? Our aim is to cut through the thick forest of information and provide you with clear answers.When do you need to see a fertility doctor? What tests do you need? What treatments are right for you? How should you choose your fertility clinic? What can you do to improve your fertility prospects? We answer these and other questions with evidence and our experience
Why am I struggling get pregnant?
There are many reasons why you may be having trouble. The most common reasons relate to eggs, sperm or the fallopian tubes. There are tests that can look for such problems. There are also other conditions that can be linked to a reduction in fertility, for example, having medical conditions such as thyroid disease or diabetes, or having gynaecological conditions such as endometriosis or fibroids in the uterus. 1 in 4 couples, however, will find all tests are normal although they still have difficulty conceiving; this is referred to as ‘unexplained infertility’.
All these potential causes of infertility can make you feel anxious. The good news is that modern fertility treatment can do a lot to address most of these problems. Fertility science and practice are advancing at a phenomenal speed, bringing answers and babies to couples struggling to conceive a pregnancy. If you have been struggling to conceive, do seek professional help, either from your general practitioner or a fertility clinic.
Why am I struggling get pregnant?
There are many reasons why you may be having trouble. The most common reasons relate to eggs, sperm or the fallopian tubes. There are tests that can look for such problems. There are also other conditions that can be linked to a reduction in fertility, for example, having medical conditions such as thyroid disease or diabetes, or having gynaecological conditions such as endometriosis or fibroids in the uterus. 1 in 4 couples, however, will find all tests are normal although they still have difficulty conceiving; this is referred to as ‘unexplained infertility’.
All these potential causes of infertility can make you feel anxious. The good news is that modern fertility treatment can do a lot to address most of these problems. Fertility science and practice are advancing at a phenomenal speed, bringing answers and babies to couples struggling to conceive a pregnancy. If you have been struggling to conceive, do seek professional help, either from your general practitioner or a fertility clinic.
How can egg problems affect my fertility?
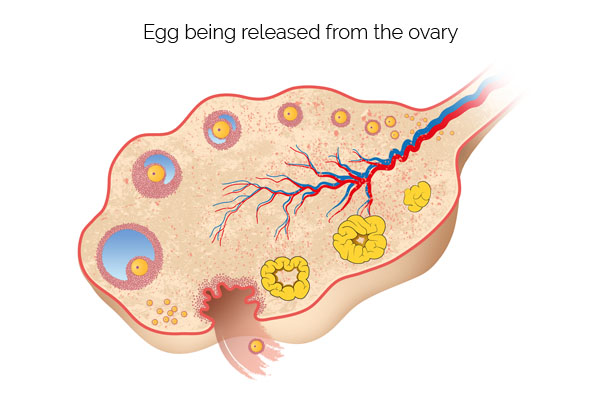
A normal ovary has a good store of eggs, and releases an egg every month. With eggs, you can have two problems. First relates to the number of eggs in the ovaries. The egg number could be very low. A woman with low number of eggs is said to have a poor ovarian reserve. It is simple to check for this condition with blood tests (FSH blood test, or ideally an AMH blood test) and a pelvic ultrasound scan to assess for the follicle count in the ovary.
The second egg problem relates to the eggs not being released from the ovaries. This is called anovulation, and it is often related to a condition called polycystic ovary syndrome. Clinical symptoms include long menstrual cycles, putting on weight, excessive body hair and acne. Simple hormone blood tests and a pelvic ultrasound scan will help diagnose polycystic ovary syndrome. A blood test, urine test or ultrasound scan can be used to check for ovulation.
How can sperm problems affect my fertility?
Sperm problems can be related to the number (or the concentration), movement (motility) or the shape (morphology) of the sperm. A sperm test will look at all three of these issues: sperm concentration needs to be more than 15million per millilitre of semen. Normal sperm motility, or movement, is when at least 40% of sperm are moving. Finally, we want at least 4% of sperm to have normal shape (normal morphology). Sometimes a sperm test may show absence of sperm.
Sometimes it may be necessary to do advanced sperm tests such as sperm DNA fragmentation assessment to unearth sperm related fertility problems.
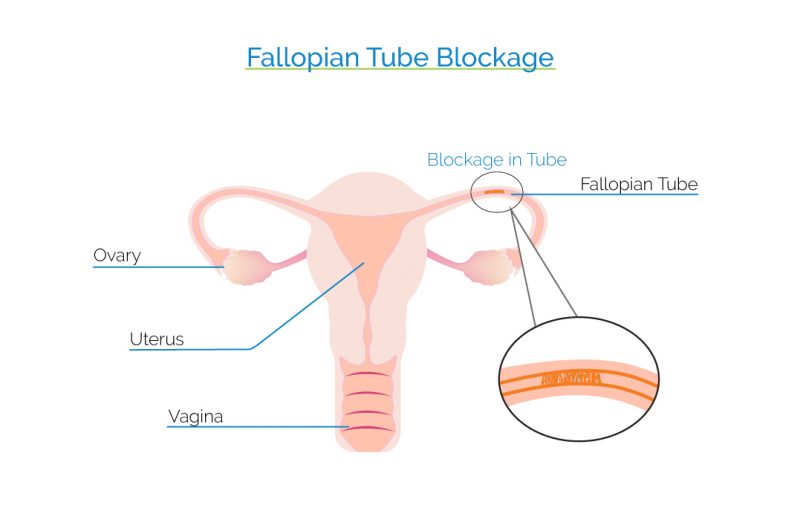
How can fallopian tube problems affect my fertility?
A fallopian tube can be blocked, or the tube lining can be damaged. We can look for blocked fallopian tubes using an ultrasound dye test called HyCoSy or an X-ray test called hysterosalpingogram. Sometimes it may be necessary to do an operation called laparoscopy which involves the surgeon inserting a camera through the belly button to fully assess the fallopian tubes with a dye test. Some blocked tubes can be treated with surgery, but for most women, IVF will be necessary.
What is the ideal frequency of intercourse and timing to improve fertility chances?
According to studies, intercourse during a six-day period leading up and ending on the day of ovulation accounts for nearly all pregnancies. The probability of conception increases as we get closer to ovulation itself. Does this mean that we can time intercourse for achieving the best chance of pregnancy? We should first remember that what works in theory doesn’t always work in practice. It can be very difficult to say exactly when the ovulation is going to take place, and therefore we cannot know with certainty when the six-day fertile window will be. Even though urinary ovulation kits and even mobile phone apps have been developed to identify the window of fertility, we know that timing of ovulation is imprecise, and trying to time the intercourse at the right time places unnecessary stress upon the couple.
So what can you do? Studies have shown that having intercourse every two or three days improves a woman’s chances of conceiving. Furthermore, regular ejaculations can help with sperm quality. So, don’t resort to techniques for finding out when ovulation is taking place, but instead aim to have intercourse two or three times a week to improve your chances of having a pregnancy.
What is the ideal frequency of intercourse and timing to improve fertility chances?
According to studies, intercourse during a six-day period leading up and ending on the day of ovulation accounts for nearly all pregnancies. The probability of conception increases as we get closer to ovulation itself. Does this mean that we can time intercourse for achieving the best chance of pregnancy? We should first remember that what works in theory doesn’t always work in practice. It can be very difficult to say exactly when the ovulation is going to take place, and therefore we cannot know with certainty when the six-day fertile window will be. Even though urinary ovulation kits and even mobile phone apps have been developed to identify the window of fertility, we know that timing of ovulation is imprecise, and trying to time the intercourse at the right time places unnecessary stress upon the couple.
So what can you do? Studies have shown that having intercourse every two or three days improves a woman’s chances of conceiving. Furthermore, regular ejaculations can help with sperm quality. So, don’t resort to techniques for finding out when ovulation is taking place, but instead aim to have intercourse two or three times a week to improve your chances of having a pregnancy.

When should I see a fertility doctor?
You should consider seeing a doctor if you have been trying for over a year. If you have certain symptoms or clinical history that may suggest a specific infertility problem, then you may want to see a doctor soon, rather than waiting for a year. Such symptoms include irregular or infrequent menstrual bleeds (particularly if your menstrual cycle length is over 35 days), painful periods, and rapid gain in body weight. If you have a clinical history of pelvic infection, fibroids or endometriosis, again you should consider seeing a doctor soon.

What tests do I need?
The female partner will need:
- a test to assess egg count in the ovaries,
- a test to see if eggs are being released from the ovaries (ovulation),
- a test for checking the fallopian tubes,
- an ultrasound scan to look for any pelvic disease.
The male partner will need:
- a semen-analysis.
What can I do to improve my prospects of success from fertility treatment?
Our short video addresses this question for IVF patients, but the principles apply to all patients who are trying to conceive a pregnancy naturally or with IVF. It is important to follow our advice on
- Diet
- Micro-nutrients
- Body mass index
- Reducing caffeine and alcohol consumption
- Sleep and stress management.
However, follow the advice with a ‘light touch’, that is to say if you lapse on some of the advice on some days, that is OK!
Are birth control pills linked to infertility?
Scientific studies show contraceptive pills, regardless of its type and duration of use, do not have a negative effect on the ability of women to conceive and do not significantly delay fertility. So, you have no reason to worry about this.
The same is true for other forms of contraception, such as birth control patches, intrauterine contraception devices and implants. None of these affects your fertility prospects. However, if you periods are not monthly after coming off a contraception, you should seek medical advice.

Can stress cause infertility?
Subfertility can impose a huge psychological burden on couples. Couples who face difficulties conceiving often face stress related to not achieving a pregnancy; some have stressful jobs or family circumstances.
The relationship between stress and subfertility has been debated for years. Couples with difficulties conceiving report elevated levels of anxiety and depression, and it is clear that infertility can cause stress. What is less clear, however, is whether or not stress causes subfertility. A precise cause-effect relationship is still difficult to demonstrate, but some studies have suggested a vicious cycle between stress and subfertility, where subfertility causes distress which in turn has an effect on the chances of conceiving a baby.
Stress doesn’t, of course, affect only the female partner. According to studies, poorer semen quality is detected among men with stress. In particular, stress can affect the sperm volume, count and concentration.
Some couples prefer to modify their lifestyle through a structured program of physical exercise, psychological support, mindfulness or acupuncture in order to reduce stress in their lives. Such programs often succeed in reducing stress and increasing the couple’s chances of conceiving. Some couples benefit from a formal counselling arrangement with a fertility counsellor.
Can stress cause infertility?
Subfertility can impose a huge psychological burden on couples. Couples who face difficulties conceiving often face stress related to not achieving a pregnancy; some have stressful jobs or family circumstances.
The relationship between stress and subfertility has been debated for years. Couples with difficulties conceiving report elevated levels of anxiety and depression, and it is clear that infertility can cause stress. What is less clear, however, is whether or not stress causes subfertility. A precise cause-effect relationship is still difficult to demonstrate, but some studies have suggested a vicious cycle between stress and subfertility, where subfertility causes distress which in turn has an effect on the chances of conceiving a baby.
Stress doesn’t, of course, affect only the female partner. According to studies, poorer semen quality is detected among men with stress. In particular, stress can affect the sperm volume, count and concentration.
Some couples prefer to modify their lifestyle through a structured program of physical exercise, psychological support, mindfulness or acupuncture in order to reduce stress in their lives. Such programs often succeed in reducing stress and increasing the couple’s chances of conceiving. Some couples benefit from a formal counselling arrangement with a fertility counsellor.
How does age affect my fertility chances?
Women are born with 1–2 million potential eggs, and by the time they reach puberty, a woman’s egg count might be around 400,000. The human body is not able to produce more eggs.
Many people think women lose just one egg per cycle, but that’s not the case. Most of the eggs that exist in a woman’s ovary are in a sleeping, or inactive, state. With each cycle a certain number of eggs is prepared for ovulation, but usually only one egg is allowed to mature and be released from the ovaries. With each cycle a woman loses about 1,000 eggs, and that loss accelerates as we get older. Around the age of 35, the decline in egg store starts to get steeper.
So, the number of eggs diminishes with the passing of time, but there is also an issue of quality. Are all eggs “equal”? Do all eggs have the same potential of creating an embryo? It seems that nature does not give the same potential to all eggs. It’s unclear whether this happens because the better quality eggs get released earlier on in the course of a woman’s life or because they accumulate genetic mutations with the passage of time that makes it more difficult for the eggs to produce healthy embryos. The fact remains that as a woman grows older, the quality of the eggs in her ovaries also decline. This is why there is an increase in pregnancy loss and chromosomal problems with advancing age.
Both natural live birth rate and IVF success is significantly lower for women in their late 30s and 40s. So, if you are struggling to conceive, it is important to seek timely help.