We now have numerous very effective fertility treatments that are giving childless couples the means to achieve their dream of having a child. Here we discuss the well-established treatment approaches as well as some of the newer but controversial ‘add-on’ treatments. You will need to have your fertility treatment in a fertility clinic; the first step in this journey is seeking a consultation with a fertility specialist.
We now have numerous very effective fertility treatments that are giving childless couples the means to achieve their dream of having a child. Here we discuss the well-established treatment approaches as well as some of the newer but controversial ‘add-on’ treatments. You will need to have your fertility treatment in a fertility clinic; the first step in this journey is seeking a consultation with a fertility specialist.
There are so many different fertility treatments. Which one is right for you? Would it be IUI, IVF, ICSI, treatment with donated sperm or eggs, or fertility surgery? The specific fertility treatment you need will depend on your clinical history, test findings and your preferences. We provide details of the various treatment options here, but make sure you look at our Fertility Journeys to get an idea about what treatments may be right for you. If you need further help, please book a consultation with us.
Ovulation induction: Clomid, Letrozole or FSH injection treatment
The purpose of ovulation induction is to help a woman release an egg from an ovary. Women with conditions such as polycystic ovary syndrome may not be releasing an egg from their ovaries, and cannot therefore become pregnant.
Pills, such as clomid or letrozole, or FSH injections can be used to make the ovary release an egg. Clomid, letrozole or FSH injection helps to develop follicles (which are fluid filled sacs containing eggs).
When one or two follicles reach a mature size (about 18 – 20mm in diameter), ovulation may occur naturally, or ovulation can be induced with a hormone called HCG (Gonasi or Ovitrelle injection). It is important to monitor the growth of the follicle with ultrasound to ensure there is there is good growth and that there aren’t too many follicles developing, which can result in multiple pregnancies and related complications.
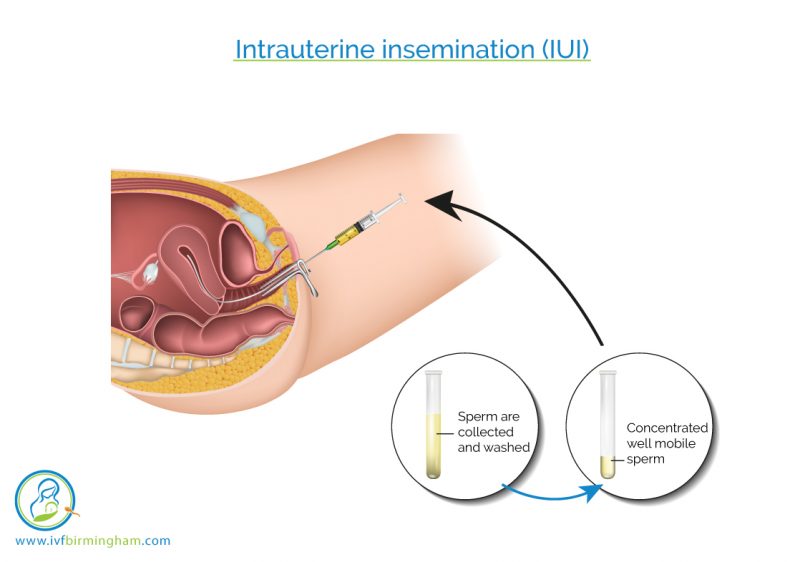
Intrauterine insemination (IUI)
The purpose of IUI is to introduce sperm into the womb cavity, just at the correct time (that is on the day before or day of ovulation). The sperm is specially prepared and concentrated. It is then loaded up into a fine plastic tube, which is then placed into the womb cavity at the correct time, and the sperm is released into the womb. IUI can be useful for couples with very slight problems with sperm concentration or movement, or for couples in whom no cause is found for infertility (‘unexplained infertility’).
IUI can be combined with ovulation induction (with clomid tablets or FSH injections). Ovulation can occur naturally or with the help of HCG hormone (Gonasi or Ovitrelle) injection. Ovulation can be monitored with ultrasound scans or with urinary LH dipsticks.
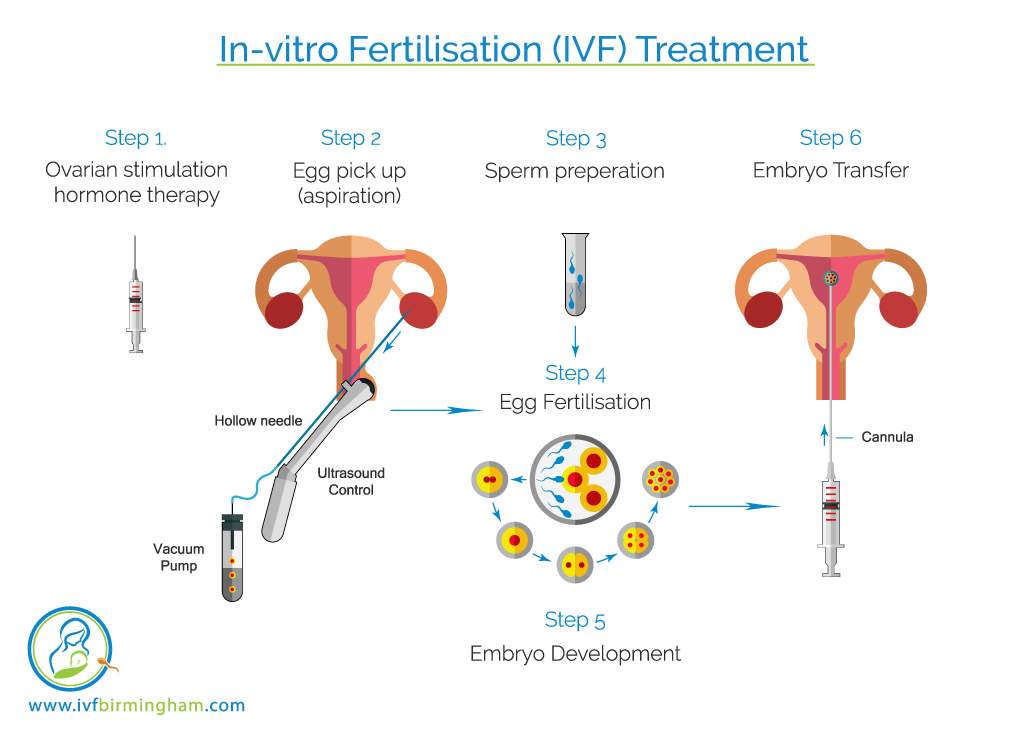
In-vitro Fertilisation (IVF) treatment
The purpose of IVF treatment is to create and grow embryos (fertilized eggs) in the laboratory, and transfer one or two embryos into the womb at the correct time (usually between days 2 to 5 of embryo development).
IVF treatment is extremely popular and a great treatment for many infertility problems. For example, it can be useful for women with anovulation (e.g. PCOS), blocked fallopian tubes, unexplained infertility and single women or same sex couples seeking donor sperm treatment.
IVF treatment is complex. Many different steps are involved and various treatment plans can be used. Details of the various steps and various treatment plans can be found on our ‘IVF companion’ page, but here is a simple infographic presentation that lays out the basic steps of IVF.
Intra-cytoplasmic sperm injection (ICSI) treatment
ICSI is the same as IVF treatment, except for one step: In ICSI the egg and sperm are brought together by injecting the sperm directly into the egg. ICSI is useful when there is problem with donor sperm concentration, movement or shape, or if there is a history of poor fertilisation of eggs in previous IVF cycles.
Surgical sperm retrieval
Surgical sperm retrieval can be performed when no sperm is seen on a sperm test. There may be no sperm because the testicle is not making sperm or because there is an obstruction not allowing the sperm to travel from the testicle in to the ejaculate. In both scenarios it may be possible to collect sperm directly from the testicle itself.
In couples where there is no sperm seen on the sperm test, a surgical sperm retrieval will be offered as a last option for the male to use their own sperm to form an embryo in ICSI treatment. The procedure involves either a local anaesthetic or general anaesthetic. The scrotum is then thoroughly cleaned and small narrow needles are then used to aspirate sperm out of different parts of the testicle. If no sperm can be collected using the needles a biopsy of the testicle can be done through small incision in the testicle.
The risks of surgical sperm retrieval are pain, bleeding, infection and blood clot formation.
If no sperm is found by surgical sperm retrieval then treatment with donated sperm may be required.
Frozen embryo transfer treatment
Many couples, following an IVF treatment, have embryos in freeze storage. These embryos can be thawed and transferred into the womb to give the couple a chance of pregnancy. Before the transfer of the embryo(s), the womb lining is grown with oestrogen tablets; once the lining has reached an appropriate thickness, progesterone pessaries are used to mature the womb lining. Once the womb lining is ready, the embryo transfer procedure is carried out with a fine plastic catheter. The procedure is not painful and there are virtually no risks with the procedure.
If there are two or more embryos in freeze storage, to maximise pregnancy rates, the best quality embryos are selected for transfer. Not all embryos survive the freezing and thawing process. Each embryo has about 90% chance of surviving. Usually one embryo is selected, to avoid multiple pregnancy and associated complications.
Donor sperm treatment
Donor sperm may be used when male partner has no sperm or for single women or female same sex relationships where there is no male partner.
Sperm donors are screened to be fit and healthy and have tests to ensure do not carry any infections or have any genetic conditions in their families. Your fertility doctor will refer you to a counsellor so that you understand the legal and emotional implications of using donor sperm for your fertility treatment. The sperm donor will also be matched to your requirements, for example, your ethnicity and hair colour.
Donor sperm may be used in IUI (intrauterine insemination), IVF or ICSI treatment. The type of donor sperm fertility treatment will depend on the circumstances of your infertility.
Donor egg treatment
Donor egg treatment may be used in a number of scenarios:
- When the store of eggs in your ovaries is too low for IVF treatment (this could be because of early menopause, surgical removal of your ovaries or general low egg store in your ovaries)
- Chemotherapy which has damaged your ovaries
- A chance that the use of your own eggs could pass on a genetic condition to your offspring.
Egg donors are usually young (less than 35 years of age) with a normal store of eggs. The egg donor can either be anonymised or someone that you know who has volunteered to give you her eggs. Like with sperm donors, egg donors are screened to ensure that they do not carry infections such as HIV or hepatitis B and C. Egg donors will also be screened to ensure that they do not have hereditary diseases in their family.
Your fertility doctor will refer you for counselling so that you are made aware of the potential legal and emotional implications of using donated eggs. The egg donor will be matched to your requirements, for example, your ethnicity and hair colour.
Use of donor eggs will require IVF treatment with the egg donor undergoing ovarian stimulation and egg collection. The embryo will then be formed and then transferred inside your womb to achieve pregnancy.
Surrogacy treatment
Surrogacy treatment is used when the female partner is unable to carry a pregnancy. This could be because the female partner has fibroids or other problems in the womb, or if she has no womb whatsoever (for instance if the womb was removed or if no womb ever developed). The ‘commissioning couple’ (the male and female partners who are using their egg and sperm to create the embryo) will undergo IVF treatment, the embryo will be created, and this embryo will then be transferred in to a surrogate female. The surrogate may be anonymous or someone that you know who has volunteered to be your surrogate.
If you need surrogacy as part of your fertility treatment, your fertility doctor will refer you to a counsellor who will discuss with you the emotional and legal implications of surrogacy treatment.
Surgical treatments for infertility
There are some causes of infertility that may be helped by an operation. The potential benefits of any operation will need be considered along with possible risks. The surgery can be on the ovary, fallopian tubes or the womb.
Ovarian surgery for infertility: If you have polycystic ovary syndrome and have not responded to tablets to help you release an egg each month, you may be offered a keyhole operation to ‘drill’ some holes in the ovary. This is called ovarian drilling, and the aim is to reset the ovaries’ hormones to try and help the release eggs. If you have endometriosis affecting your ovaries, you may be offered an operation to have endometriotic cysts removed from the ovary.
Tubal surgery for infertility: If you have blocked and fluid-filled fallopian tubes (called hydrosalpinges), your IVF doctor may suggest that you could have a key-hole operation to try and have this fixed. Sometimes this could be an operation to try and correct the blockage and sometimes it may be better for the tubes to be removed.

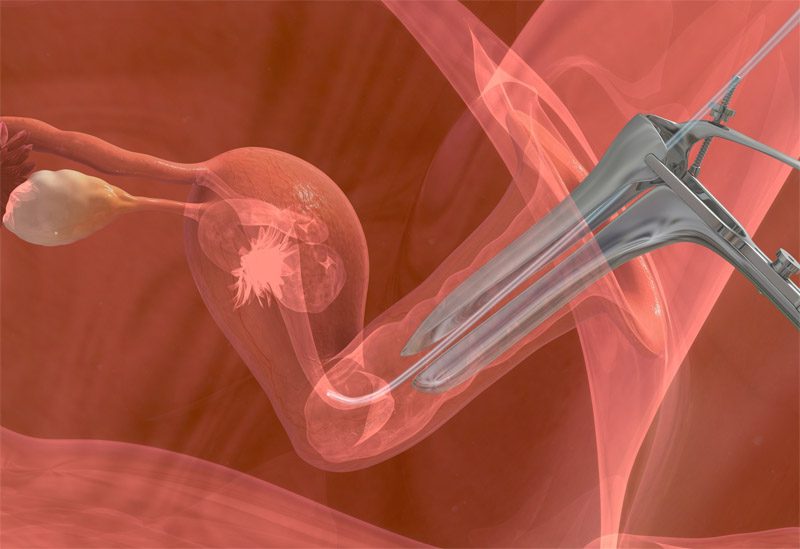
Uterine surgery for infertility: If you have a fibroid, polyp or septum inside your womb, this can affect how a pregnancy implants to the lining of the womb. Sometimes, your IVF doctor may suggest that the polyp or fibroid be removed using a hysteroscopy (a camera test inside your womb) procedure. If you have many or large fibroids, it may be necessary to have a bigger operation with an open cut on your abdomen to remove the fibroids.
What are add-on treatments?
Patients and their doctors constantly look for ways to improve the chances of success with IVF treatment. This is particularly the case for women who may have had one or more unsuccessful IVF treatment cycles already. For such women, add-on treatments to improve fertilisation, embryo development, endometrial receptivity and pregnancy rates are often considered. However, such treatment needs to be based on evidence. We review the evidence and provide our recommendations here. However, you should discuss the specific details of your clinical care with your own fertility specialist doctor. You can also look at the HFEA website for their view of the add-on treatments. If you wish to discuss any of the add-on treatments, please book a consultation with us.
Evidence for add-ons:
The importance of randomised controlled studies (RCTs)
Evidence on the effectiveness of an add-on treatment can come from difference types of research studies. From amongst the various types of studies, a Randomised Controlled Study, or an RCT for short, is the most reliable source of evidence. We have used RCTs as the source of evidence in our discussions below. If there are more than 1 RCT showing the same or similar finding, our confidence in the finding would by high. If the RCTs show conflicting evidence, then our confidence in the finding would be low. If there is only limited evidence from RCTs, we have relied on non-RCT evidence, but we have kept this to a minimum.
Human Fertilisation and Embryology Authority (HFEA) has proposed a traffic light system to grade the evidence on add-on. They propose a green symbol where there is more than one good quality RCT which shows that the procedure is effective and safe. They propose an amber symbol where there is a small or conflicting body of evidence, which means further research is still required and the technique cannot be recommended for routine use. Finally, a treatment is graded red if there is no evidence to show that it is effective and safe.
Research is so important for making discovering and finding out if interventions actually bring any benefit to patients. We have made huge progress in medicine and IVF only because women and men took part in research in the past. We encourage you to take part in research studies, particularly RCTs, so that you can contribute to improving care and outcomes.
EmbryoGlue
What is it?
EmbryoGlue is an adherence compound called hyaluronic acid that is added to the fluid (medium) containing the embryo during transfer to the womb cavity. It is intended to help with implantation of the embryo(s) to the lining of the womb (endometrium)
What is the evidence?
Hyaluronic acid has been studied in 16 randomised control trials, with over 3000 participants. The synthesized evidence from the studies found a 39% relative increase in pregnancy rate and 41% relative increase in live birth rate with this add-on treatment. There was also an increase in the number of multiple pregnancies with this treatment.
What is our recommendation?
There is substantial evidence suggesting benefit from this treatment. It is worthwhile considering adding Embryo Glue to your IVF treatment.
Scientific Research Summary
EmbryoGlue
What is it?
EmbryoGlue is an adherence compound called hyaluronic acid that is added to the fluid (medium) containing the embryo during transfer to the womb cavity. It is intended to help with implantation of the embryo(s) to the lining of the womb (endometrium)
What is the evidence?
Hyaluronic acid has been studied in 16 randomised control trials, with over 3000 participants. The synthesized evidence from the studies found a 39% relative increase in pregnancy rate and 41% relative increase in live birth rate with this add-on treatment. There was also an increase in the number of multiple pregnancies with this treatment.
What is our recommendation?
There is substantial evidence suggesting benefit from this treatment. It is worthwhile considering adding Embryo Glue to your IVF treatment.
Scientific Research Summary
Artificial egg activation (AOA)
What is it?
In couples with previous fertilisation failure, artificial oocyte activation (AOA) with mechanical, electrical or chemical stimuli may help to achieve fertilisation of the eggs after ICSI treatment, giving the couple a chance of pregnancy.
What is the evidence?
AOA has been studied in 9 randomised trials, with 2 studies studying women, with 168 participants, and 7 studies evaluating eggs, with a total of 4234 eggs. The studies found AOA resulted in more fertilised eggs (8 fold increase) and more embryos (5 to 10 fold increase). However, as the studies were small and of poor methodological quality and there was statistical uncertainty in some of the results, we cannot make a firm conclusion about the results.
What is our recommendation?
We cannot make a firm recommendation for or against AOA, although it may have some benefits in selected groups of patients. We advise you to discuss the evidence with your fertility specialist.
Scientific Research Summary
Steroids (e.g. prednisolone)
What is it?
Steroids, such as prednisolone, are thought to improve the lining of the womb and increase the chances of implantation of the embryo, by modulating immune activity.
What is the evidence?
Steroids have been studied in 14 randomised trials, involving 1,879 participants. The overall synthesized evidence did not find an improvement in pregnancy or live birth rate. However, when the IVF studies and ICSI studies were separately reviewed and synthesised, IVF studies showed a 50% relative increase in pregnancy rate with steroid use (6 studies with 650 participants contributed to this analysis). This is an interesting finding! ICSI is performed for male (sperm) problems, and therefore in the ICSI studies, there is no reason to expect a preponderance of female immune problems; however, in the IVF studies, where there is no male problems, one can expect a pre-ponderance of female problems, some of which may be an immune problem. So, seeing some benefit in the IVF studies where there is an ‘enrichment’ of female infertility problems makes biological sense. Women with an identified immune problem may be expected to benefit most from steroid treatment; The researcher Litwicka and colleagues put this idea to test in a randomised trial of 60 patients with thyroid antibodies (an immune problem), and found high clinical pregnancy and live birth rates with steroids (pregnancy rate in the prednisolone group was 46.6%, and in the control group it was 16.6%).
What is our recommendation?
Steroid treatment is associated with potential risks, so it is very important to be clear about the pros and cons before going ahead with taking a course of steroids during IVF treatment. We think steroids may have a role only in patients with an immune problem, for example those with auto-antibodies, but the available evidence is not enough for us to make a strong recommendation.
Scientific Research Summary
Steroids (e.g. prednisolone)
What is it?
Steroids, such as prednisolone, are thought to improve the lining of the womb and increase the chances of implantation of the embryo, by modulating immune activity.
What is the evidence?
Steroids have been studied in 14 randomised trials, involving 1,879 participants. The overall synthesized evidence did not find an improvement in pregnancy or live birth rate. However, when the IVF studies and ICSI studies were separately reviewed and synthesised, IVF studies showed a 50% relative increase in pregnancy rate with steroid use (6 studies with 650 participants contributed to this analysis). This is an interesting finding! ICSI is performed for male (sperm) problems, and therefore in the ICSI studies, there is no reason to expect a preponderance of female immune problems; however, in the IVF studies, where there is no male problems, one can expect a pre-ponderance of female problems, some of which may be an immune problem. So, seeing some benefit in the IVF studies where there is an ‘enrichment’ of female infertility problems makes biological sense. Women with an identified immune problem may be expected to benefit most from steroid treatment; The researcher Litwicka and colleagues put this idea to test in a randomised trial of 60 patients with thyroid antibodies (an immune problem), and found high clinical pregnancy and live birth rates with steroids (pregnancy rate in the prednisolone group was 46.6%, and in the control group it was 16.6%).
What is our recommendation?
Steroid treatment is associated with potential risks, so it is very important to be clear about the pros and cons before going ahead with taking a course of steroids during IVF treatment. We think steroids may have a role only in patients with an immune problem, for example those with auto-antibodies, but the available evidence is not enough for us to make a strong recommendation.
Scientific Research Summary
Endometrial scratch
What is it?
Endometrial ‘scratch’, which is intentional damage to the lining of the womb with a plastic catheter, was believed to rejuvenate the lining, and improve the chances of embryo implantation in the womb.
What is the evidence?
Endometrial scratch has been studied in 15 randomised clinical trials, with over 3900 participants. There were differences in the time and the way the researchers did the endometrial scratch, as well as the specific patients they studied (e.g. in some studies, it was couples having the first cycle of IVF, and in others, it was couples with previous unsuccessful cycles). The findings from the earlier studies, which were of limited quality, were that there was an increase pregnancy rate and live birth with endometrial scratch. However, unfortunately, a comprehensive synthesis of all the evidence in 2019 did not find any improvement in pregnancy or live birth rate with endometrial scratch treatment. This was further confirmed in a recent high quality study which did not find any benefit at all from this procedure; this study studied a total of 1364 participants, and found that the live birth rate in the scratch group was 26.1%, and in the comparison group, it was again 26.1%, showing absolutely no benefit whatsoever. A large UK study is due to report its findings soon.
Intralipids
What is it?
Intralipid is a fat emulsion made from soybean oil, glycerine and egg. It can reduce inflammation and natural killer cell activity, prompting researchers to consider its role in addressing immune problems in reproduction.
What is the evidence?
Intralipids have been studied in 2 randomised trials, including a total of 398 participants.
First Study
Researcher Dakhly and colleagues studied 296 women with unexplained infertility or recurrent miscarriage and elevated levels of natural killer cells (>12%) who were given either intralipid or saline infusion.
Live birth rate was 37.5% in the intralipid group versus 22.4% in the control group.
Second Study
Researcher Singh and colleagues studied 102 women with previous unsuccessful IVF or ICSI treatment; half the women were given intralipid and the other half were given saline infusion.
Pregnancy rate was 34.6% in the intralipid group versus 14% in the control group.
What is our recommendation?
We think intralipids may have a role only in patients with an immune problem, for example those high levels of natural killer cells, but the available evidence is not enough for us to make a strong recommendation
Scientific Research Evidence
Intralipids
What is it?
Intralipid is a fat emulsion made from soybean oil, glycerine and egg. It can reduce inflammation and natural killer cell activity, prompting researchers to consider its role in addressing immune problems in reproduction.
What is the evidence?
Intralipids have been studied in 2 randomised trials, including a total of 398 participants.
First Study
Researcher Dakhly and colleagues studied 296 women with unexplained infertility or recurrent miscarriage and elevated levels of natural killer cells (>12%) who were given either intralipid or saline infusion.
Live birth rate was 37.5% in the intralipid group versus 22.4% in the control group.
Second Study
Researcher Singh and colleagues studied 102 women with previous unsuccessful IVF or ICSI treatment; half the women were given intralipid and the other half were given saline infusion.
Pregnancy rate was 34.6% in the intralipid group versus 14% in the control group.
What is our recommendation?
We think intralipids may have a role only in patients with an immune problem, for example those high levels of natural killer cells, but the available evidence is not enough for us to make a strong recommendation
Scientific Research Evidence
DHEA or testosterone treatment
What is it?
Treatment with male hormones such as dehydroepiandrosterone (DHEA) or testosterone is thought to improve the egg numbers in women known to have reduced egg store in the ovaries.
What is the evidence?
DHEA has been studied in 12 randomised trials (1246 participants) and testosterone has been studied in 4 randomised trials (345 participants). The synthesised evidence from the DHEA studies did not give a clear answer, as some studies suggested benefit whilst others did not show any benefit. However, the 4 studies on testosterone treatment suggested more than doubling in chance of live births. There is a high quality randomised trial on testosterone underway at the moment, and this should give us further evidence.
What is our recommendation?
As the evidence from the DHEA studies have not produced a clear answer, we would not recommend this treatment. Testosterone, on the other hand, may have benefits in women known to have reduced egg store, and may be worthy of consideration. We cannot, however, make any firm recommendations until we have further randomised trial evidence.
Scientific Research Summary
Heparin (LMWH – Low Molecular Weight Heparin)
What is it?
Heparin, which can go by various trade names such as Clexane, Fragmin and Inhixa, is a blood-thinning drug. It may also improve the condition of lining of the womb and thereby help with implantation.
What is the evidence?
Heparin has been studied in 3 randomised trials, involving 386 participants. The study participants varied in that one study included women having their first IVF cycle, with no blood clotting disorders, the second study included women with at least one blood clotting disorder, and the third included women who had undergone at least two previous unsuccessful ART cycles. The synthesised evidence from the 3 studies found a 61% relative increase in pregnancy rate and a 77% relative increase in livebirth rate.
What is our recommendation?
We think it is worthwhile considering heparin treatment if you have been found to have a ‘sticky blood disorder’ or you have had multiple unsuccessful IVF or ICSI cycles despite having transfers of good quality embryos.